How Microbes Moved From Villain to Hero
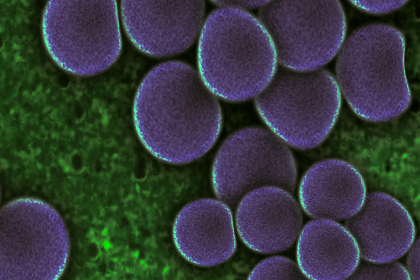
Microbes live inside all of us. The idea of a "microscopic menagerie" teeming and thriving in your cells, your intestines and your brain might make you a little uncomfortable, but this is good news, according to the latest science.
U.K.-based science writer Ed Yong says microbiomes — the fungi, bacteria, viruses and other minuscule critters — are necessary "partners" for the betterment of our immune systems.
August 22, 2016 | Source: Mercola.com | by Dr. Joseph Mercola
Microbes live inside all of us. The idea of a "microscopic menagerie" teeming and thriving in your cells, your intestines and your brain might make you a little uncomfortable, but this is good news, according to the latest science.
U.K.-based science writer Ed Yong's new book, "I Contain Multitudes: The Microbes Within Us and a Grander View of Life," says microbiomes — the fungi, bacteria, viruses and other minuscule critters — are necessary "partners" for the betterment of our immune systems.
Your microbiomes change constantly, and what you eat makes a big difference in the kind of microbes your body contains. When people begin improving their diets, the number and integrity of their microbes improve. In fact, through your diet, you can, to a degree, switch them out, Yong asserted:
"It seems that dietary fiber is a really important driver of microbial diversity in our bodies. Fiber consists of large numbers of different carbohydrates — many we can't digest, but our bacteria in our guts can. If we eat low-fiber diets, we narrow the range of our microbial partners.
Simple measures like probiotics — adding a few strains of microbes in the hope that they will take hold and remedy health problems — have been largely unsuccessful. It will take more
… If we want to add microbes to our bodies, we'll need to think about whether we need to eat certain foods to nourish the microbes we're taking."1
Human gut bacteria may have existed for millions of years, maybe before the evolution of people.
A recent study asserts that three types of gut bacteria affected intestinal development, fought off germs and may have influenced mood and behavior and were reportedly present in African great apes that lived more than 10 million years ago.
Scientists believe the bacteria "evolved into distinct strains as humans and great apes went their separate evolutionary ways." Study authors hope similar gut microbes can be eventually traced past amphibians and even vertebrates.2
How Science Approaches 'Fixing' Broken Microbiome Function
While microbiome science is still in the early stages, scientists have explored why certain foods are good for us and others aren't. The connection between food, microbes and health are all inextricably intertwined, and unraveling the mysteries may shed light on how they affect our metabolism.
Fiber, for instance, is good for many of our gut bacteria, so eating more veggies certainly won't hurt. Microbiome researcher Jeff Leach told NPR3 that too little might starve the good bacteria, and "when we starve our bacteria they eat us. They eat the mucus lining — the mucin in our large intestine."
Fiber feeds your bacteria and gives off nourishing nutrients for your gut lining. Veggies are high-fiber foods, so eating a variety and as much of the whole thing as possible is recommended.
Garlic and onions also have antimicrobial properties; garlic impairs some of the undesirable bacteria but leaves the good ones. As Leach explained:
"Those vegetables contain high levels of a type of fiber called inulin, which feeds actinobacteria in our guts. In fact, inulin is considered a probiotic, since it feeds the good bacteria, or probiotics, that live inside us."
He added that slight or short-term diet tweaks may not make much of a difference in gut health, but moving from ingesting 10 to 15 grams of fiber a day to more like 40 or 50, "you may see some changes."
The Gut-Brain Axis: How Your Brain Influences Hunger
Scientists at Rockefeller University used magnetic stimulation in the ventromedial hypothalamus part of the brains of genetically engineered mice to "switch on" neurons to see how the brain might influence appetite. According to Scientific American, they found that the procedure:
"Increased the rodents' blood sugar levels and decreased levels of the hormone insulin. Turning on the neurons also caused the mice to eat more than their control counterparts …
They inhibited these neurons and saw the opposite effects: it drove blood sugar down, elevated insulin levels and suppressed the animals' urge to consume their chow."4
Scientists have been aware for over a century that the brain "talks to the mind" through nerve connections, as well as biochemical signals such as hormones, to affect metabolism in a connection called the "gut-brain axis."
Studies have concentrated on the communication pathways between the nervous and digestive systems to treat metabolic disorders, especially since obesity and metabolic disease is increasing steadily worldwide.
Four in 10 women in the U.S. are considered obese5 and diabetes prevalence has almost quadrupled since 1980, so scientists and pharmaceutical companies are working on the gut-brain link with increased urgency to devise drugs, surgery, devices and probiotic approaches.
In 2011, Dr. Serguei Fetissov from Rouen University in France started his company TargEDys to develop treatment programs for metabolic disorders and conducted mice studies using Escherichia coli (E. coli) intestinal bacteria to reduce their appetite. Scientific American reported:
"Fetissov is trying to replicate these effects in the rodents by using a probiotic to hasten the proliferation of E. coli and boost production of appetite-reducing proteins, rather than by administering injections of the bacterial protein products."6
Early in 2016, TargEDys announced plans for clinical trials using freeze-dried probiotic bacteria in capsule form to use on humans and hoping to replicate the appetite-suppressing effects seen in the mice trials. Similarly, a potential therapy for anorexia patients or elderly involves bacteria to stimulate hunger.
